ASTMH 2018, Ashenafi Assefa: “Ethiopia: Assessment of malaria transmission dynamics using multiplex serological assay”
Collaborator(s): Ethiopian Public Health Institute (EPHI), Ethiopia
Countries: Ethiopia
Published: 29/10/2018
In collaboration with ASTMH, Image Audiovisuals, and session presenters, MESA brings you this webcast from the 67th ASTMH annual meeting in New Orleans, October 2018
Title: “Ethiopia: Assessment of malaria transmission dynamics using multiplex serological assay “
Speaker: Ashenafi Assefa, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Session information:
October 29, 2018, 10:15 AM – 12:00 PM, Marriott – Sheraton – Rodrigue Gallery (1st Floor)
Abstract:
Serological methods are increasingly utilized to estimate malaria transmission in low transmission settings. Malaria burden measures using conventional diagnostic methods in cross-sectional household surveys may incompletely detect the intensity and pattern of malaria transmission over time. This study describes the seroprevalence and pattern of malaria transmission in Ethiopia.
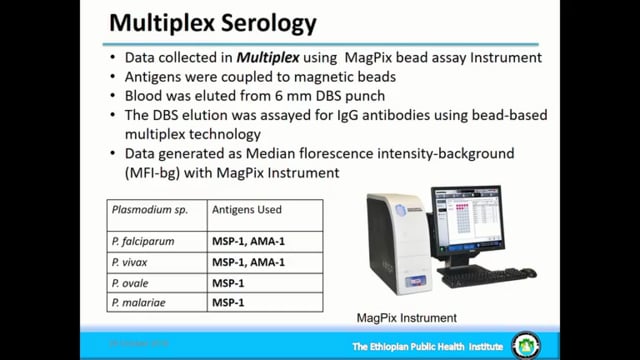
Dried blood spot (DBS) samples collected during the Malaria indicator Survey 2015 representing malarious areas of Ethiopia were analysed with bead-based multiplex assays for IgG antibodies to 12 Plasmodium spp. antigens. Species-specific responses to MSP1 antigens were used to estimate the seroprevalence for the four human malaria species (P. falciparum, P. vivax, P. malariae and P. ovale). Frequency of seropositivity and seroconversion rates were fitted to models stratified by altitude and administrative regions.
Of 8045 DBS samples collected, 7961 serological results were available for analysis. The mean age of participants was 14.8 years (95% CI: 14.7-17.3); 4197 (52.7%) participants were female. National seroprevalence was 26.4 % (95% CI: 25.5-27.5) for P. falciparum and 20.6% (95% CI: 19.7-21.5) for P. vivax. Estimated seroprevalences for P. malariae and P. ovale were 3.7% (95% CI: 3.3-4.2) and 1.1% (95% CI: 0.9-1.4), respectively. Seroprevalences were higher at lower altitudes (<2000m) compared to higher altitudes (2000-2500m); OR 2.2 (95% CI: 1.8-2.6) and 1.3 (95% CI: 1.1-1.6) for P. falciparum and P. vivax, respectively. Among Regions, the P. falciparum seroprevalences ranged from 41.4% (95% CI: 36.3-46.8) in Benishangul-Gumuz to 3.6% (95% CI: 0.9-13.3) in Harari Region. For P. vivax, the seroprevalence ranged from 37.0% (95% CI: 33.7-40.3) in Amhara to 3.1% (95% CI: 2.0-4.6) in Somali Region. Models fitted to measure transmission patterns show variability by regions, antigen type and within species.
Using serology, this study explored the cumulative malaria burden in Ethiopia and the use of multiplex assay on multiple antigens in a low transmission setting as a more sensitive biomarker using samples collected in a national survey.
THEMES: Measurement of Transmission | Surveillance