Keystone Symposia “The Malaria Endgame” – 2019: Day 2
Thursday, 31st October 2019
Published: 31/10/2019
This report is brought to you by the MESA Correspondents Solomon M. Abay, and Maya Fraser. Senior editorial support has been facilitated by Hannah Slater (PATH) and Flaminia Catteruccia.
THEMES: THEMES: Basic Science | Epidemiology | Health Systems
MESA Correspondents bring you cutting-edge coverage from the Keystone Symposia “The Malaria Endgame: Innovation in Therapeutics, Vector Control and Public Health Tools”
Day 2: Thursday, 31st October 2019
Welcome and Keynote Address
Participants were welcomed to Day 2 of the Keystone Symposia by the conference organizers. Thierry T. Diagana (Novartis Institute for Tropical Diseases, USA) celebrated that participants came from over 40 countries. Philip Welkhoff (Bill & Melinda Gates Foundation) expressed his hope that this conference would allow people to find shared solutions to common problems across different contexts. Finally, Flaminia Catteruccia (Harvard T.H. Chan School of Public Health, USA) made special note of all the young researchers attending the conference (a third of the participants), and encouraged them to share their ideas and take advantage of social networking at the conference.
The keynote talk addressed a prominent emerging technology in the world of malaria control: gene drives for vector control. Stephanie L. James (Foundation for the National Institutes of Health, USA) discussed how gene drive technology could be implemented given the regulatory, ethical, and engagement hurdles that pose such a significant challenge. A diverse working group recently published guidelines that built upon the WHO’s recommendations for ethical gene drive development. The overall message stressed engagement with stakeholders, communities, and regulators throughout all the development process. Transparency is also key to gain acceptance and support. She predicted that public mistrust is the single greatest threat to the development and ultimate deployment of this potentially game-changing technology.
Defeating Resistance I:
Chanaki Amaratunga (Mahidol Oxford Tropical Medicine Research Unit, Thailand) presented on Triple Artemisinin Combination Therapies (TACT). In 2007 and 2008 in some areas of Southeast Asia, studies observed delayed in parasite clearance in patients taking artemisinin based therapies. High treatment failure rates are now being reported in Cambodia, Thailand and Vietnam. She gave an overview of potential options to tackle malaria treatment failure associated with resistance, among which is the use of triple ACTs. In the Tracking Resistance to Artemisinin Collaboration II (TRAC II) project, her team revealed that the different TACTs tested were efficacious, safe and tolerable in adults infected with drug resistance parasites. Chanaki is now leading the Development of Triple Artemisinin-Combination Therapies (DeTACT) project, a randomized controlled trial comparing safety, tolerability and efficacy of two TACTs in Africa and Asia. She also highlighted the need to make this effort multidisciplinary, including bioethics, mathematical modeling, and market positioning components in the research that can highlight regional factors and speed up widescale deployment.
Wiweka Kaszubska (Medicines for Malaria Venture, MMV, Switzerland) introduced MMV as an initiative to discover, develop and deliver malaria medicines. She presented the target product profiles for treatment and prevention of malaria. Approaches to mitigating drug resistance include working on already-approved market products, examining potential drug combinations, and new drug candidates. One of these outcomes is a new ACT product, pyronaridine-artesunate, that has been developed to be used in areas where other ACTs are failing due to multiple drug resistance. She also stressed the need to understand resistance mechanisms using genotype, ex-vivo phenotype and clinical outcomes in drug selection for development.
Elizabeth A. Winzeler (University of California San Diego, USA) presented the Malaria Drug Accelerator (MaIDA), a consortium of 14 research labs that are working together to develop new types of drugs. A direction of research coming out of her lab is the use of a longer-than-typical assay to identify new compounds with a delayed killing effect. Overall, her lab has found that similarities in compound structure are associated with similar mechanisms of action. Her lab has also worked to identify resistance mutations through the use of in vitro evolution showing similar results to in vivo experiments.
Rounding out the session, Geoffrey Ian McFadden (University of Melbourne, Australia) asked the audience if we could design “genetic traps” for drug resistant mosquitoes. Malaria parasites are exposed to a radically different environment when they are taken up by the mosquito. This change in fitness landscape, especially when switching from drug pressure to absence of drug pressure, can be used to minimize the spread of drug resistance. The mutations conferring resistance to certain drugs may be advantageous in the human blood stage, but can become disadvantageous in the parasite mosquito stages, with infected mosquitoes developing fewer oocysts and sporozoites and thus being less infectious. This means the resistant parasite is less likely to be transmitted onwards. These drugs may be useful as combination partners to protect the efficacy of the primary compound.
Defeating resistance II
The second drug resistance session began with a quick round-up of work being done in Manu Prakash’s lab at Stanford University, USA. The overall goal of his work is to enhance scientific tools, focusing on low-cost designs, such as a $1 foldable microscope, and also on technology that can be deployed on a flip phone. One such app allows people around the world to identify mosquito species by the sound they make. Another technology uses spectroscopy to identify parasites, reducing the human resources necessary for microscopy. This modular microscope can also be adapted for use in diagnostics for other diseases, and they are currently looking for field sites. Contact the Prakash lab if you are interested in using or testing any of these technologies in the field.
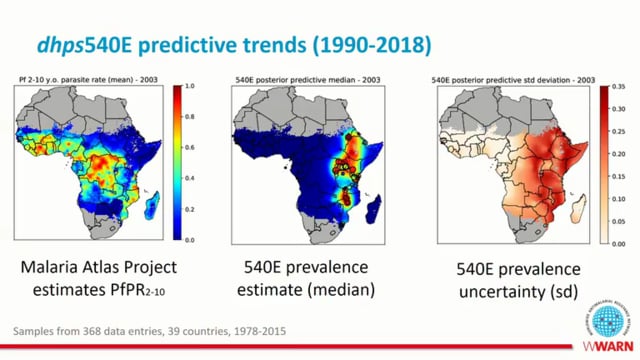
Abdoulaye Djimde (University of Science, Techniques and Technologies, Mali), presented on the status of artemisinin resistance in sub-Saharan African countries. He highlighted the origin of artemisinin resistance in Southeast Asia and updated the audience on the methods to detect artemisinin resistance, both in vivo and by molecular methods. He presented the outcome of a study conducted in Mali in 2010-2011 assessing the efficacy of a 7-day artesunate monotherapy that had adequate clinical response. His team also continued to assess responses to the same regimen in 2015 in two sites, including the previous site used during 2011. They found that at the newly added study site, patients had much slower parasite clearance. He suggested that the difference in parasite clearance time between the two villages was not related to K13 mutations as none were found in either site. He concluded his presentation by mentioning that artemisinin-based therapy is still efficacious and slow parasite clearance time in Africa is not associated with K13 mutations.
Gordon A. Awandare (University of Ghana) reminded us that P. falciparum and P. vivax are not the only parasite species out there. P. malariae and P. ovale are poorly studied and are becoming more important. His PhD student, Felix Ansah, found that using cooperative primers led to improved detection of both species even at very low parasitemia, allowing for better detection of mixed infections. With improved detection, it appears that prevalence may be higher in areas of Ghana than previously reported. He also found that parasite clearance for P. ovale and P. malariae after treatment with ACTs is slower than for P. falciparum.
Charles Wondji (Liverpool School of Tropical Medicine, UK and Centre for Research in Infectious Diseases – CRID, Cameroon) presented on molecular genetics of insecticide resistance in different Anopheles populations. He remarked that the rebound of malaria coincided with the growing insecticide resistance in 2015 and described the need for urgent insecticide resistance management. His research team focuses on understanding metabolic resistance mechanisms in major malaria vectors and their impact on mosquito fitness and Plasmodium transmissibility. He noted the way forward for insecticide-based vector control that includes: 1) Detection of molecular markers of resistance improves the detection of resistance, 2) Prioritization shall be given to keep the current Long-Lasting Insecticidal Nets (LLINs) viable, 3) Resistance management should be proactive, and 4) Use of insecticide could be complemented with novel technology, such as the genetic manipulation of insects to block their ability to transmit disease.
Lemu Golassa (Addis Ababa University, Ethiopia) closed out the session with a discussion around the detection of asymptomatic and low parasite density infections with the available tools. He showed that ultra-sensitive Rapid Diagnostic Tests (u-RDTs) are more effective than traditional RDTs at detecting low-density infections. qPCR is the most sensitive diagnostic tool, followed by loop mediated isothermal amplification (LAMP).
This report is brought to you by the MESA Correspondents Solomon M Abay (University of Addis Ababa, Ethiopia) and Maya Fraser (PATH). Senior editorial support has been facilitated by Hannah Slater (PATH) and Flaminia Catteruccia (Harvard T.H. Chan School of Public Health). This report is cross-posted on the MESA website, the Keystone Symposia Keypoint Blog and on MalariaWorld.
Published: 31/10/2019
This report is brought to you by the MESA Correspondents Solomon M. Abay, and Maya Fraser. Senior editorial support has been facilitated by Hannah Slater (PATH) and Flaminia Catteruccia.
THEMES: Basic Science | Epidemiology | Health Systems