69th ASTMH Virtual Annual Meeting – 2020: Day 2
Monday, 16th November 2020
Published: 18/11/2020
This report is brought to you by the MESA Correspondents Busari Lateef Oluwatoyin, Jaipal Singh, Nathalie Amvongo Adjia, Manuela Runge, Ivan Mbogo, Núria Balanza, Nutpakal Ketprasit, Rebecca Pwalia, Lilian Mbaisi, Ntui Vincent Ntui-Njock, and Jenna Zuromski. Senior editorial support has been facilitated by the Organizers and Co-Chairs of the symposia, Valentina Mangano and Julie Chaccour.
THEMES: THEMES: Basic Science | Epidemiology | Health Systems
MESA Correspondents bring you cutting-edge coverage from the virtual ASTMH 2020 Annual Meeting
Day 2: Monday, 16th November 2020
Symposium #3: Can We Ignore “Asymptomatic” Low-Density Malaria Any More?
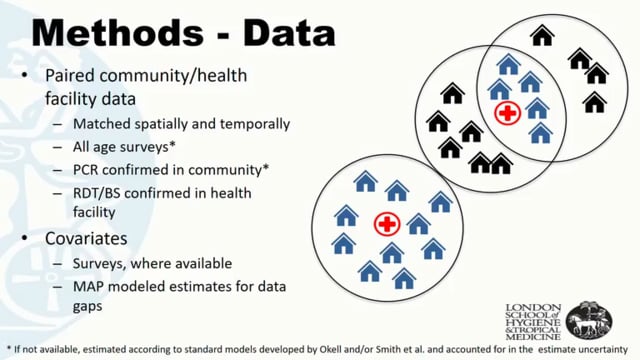
Lucy Okell (Imperial College London, United Kingdom) presented studies to highlight that detecting low-density malaria infections and identifying what factors drive infection in asymptomatic individuals are important elements in malaria elimination. Several studies have shown that low-density infections, undetectable by microscopy, are common in both P. falciparum and P. vivax. These low-density infections require ultrasensitive assays, e.g. qPCR, to be detected. Okell examined the relationship between the past and current transmission intensity in determining the relative abundance of submicroscopic infections in Africa and highlighted that low-density infections prevail in low-transmission areas. Explanations for this latter observation include 1) differences in the age distribution of infected populations with higher prevalence of infection being observed in older age groups in low transmission compared to high transmission settings; 2) low genetic diversity of the parasite in low-transmission settings favouring acquisition of protective immunity in the human population; 3) lower between parasite strains of low-transmission areas, where evolution may favour chronic low-density infections, reducing the parasite’ chances of causing symptoms that require treatment.
Dylan R. Pillai (University of Calgary, Canada) presented work on the changing landscape of malaria diagnostics. For many years, microscopy has been the gold standard for detecting malarial infection, but it comes with various limitations. Rapid diagnostic tests (RDTs) based on immunochromatographic detection of the histidine-rich protein (Hrp) have therefore played a key role in the last two decades. However, the emergence of Hrp2-deleted strains of P. falciparum limits the sensitivity of RDTs. Real-time polymerase chain reaction (PCR) emerged as a far more sensitive and specific tool to detect malaria parasites. PCR is however expensive and may not be applicable in low-income endemic areas. Recently, faster, cheaper and easier to perform loop-mediated isothermal amplification (LAMP) methods have been developed for malaria diagnosis, showing a limit of detection (LOD) of around 0.1 parasites per microliter. Also, it is possible to adapt in-house LAMP protocols enabling visual detection of samples’ positivity, therefore not requiring using of fluorescence readers. Comparison of results obtained with LAMP and qPCR show similar sensitivity of the two methods both in non-endemic and endemic areas. In non-endemic areas, the high negative predictive value of LAMP methods allows to use it as a screening test, with no further examination needed for LAMP negative samples. In endemic areas, LAMP has proven useful in detecting low-density malaria infections in pregnant women, the treatment of which resulted in improved pregnancy outcomes in clinical trials.
Though often ignored, asymptomatic low-density malaria infection plays a crucial role in maintaining transmission of the disease, presenting a setback to global malaria elimination. Gilles Cottrell (Institute of Research for Sustainable Development, France) gave a presentation on the clinical effects of low-density malaria, which often goes undetected (submicroscopic) and causes asymptomatic malaria persisting from a few days to months. Asymptomatic infection could be beneficial by decreasing the risk of malaria illness. However, it also causes anaemia in children and expectant mothers, and moreover, it is associated with low birth-weight. Furthermore, in low-transmission settings, pregnant women are at increased risk of malaria, spontaneous abortions, stillbirths and premature births. Cottrell illustrated that submicroscopic prevalence is higher than microscopic prevalence in pregnant women, with the highest prevalence being detected during the first trimester. Additionally, intermittent preventive treatment in pregnancy (IPTp) does not fully prevent malaria infections, especially submicroscopic low-density infections. Women infected before conception are at higher risk of infection during their pregnancy and maternal infection increases infants’ susceptibility to malaria. Therefore monitoring during the early pregnancy period, or even before conception, is vital for optimal protection of both women and infants. Cottrell envisaged the importance of carrying out longitudinal studies of malaria infection using highly sensitive diagnostic tools to fill the knowledge gaps in low-density asymptomatic malaria.
Fitsum Tadesse (Armauer Hansen Research Institute, Addis Ababa, Ethiopia) illustrated the relationship between asymptomatic malaria and parasite density distributions, gametocyte densities and malaria transmissibility. Especially in low-transmission settings, a large proportion of all malaria infections can be submicroscopic. Moreover, different Plasmodium species produce gametocytes at different rates: P. vivax produces them within 2-3 days, whereas P. falciparum takes 9-12 days. A study with 298 mosquito membrane feeding experiments demonstrated that infectivity positively correlates with parasitemia and gametocytemia. In humans, however, parasitaemia, gametocytemia and mosquito infectivity are correlated in asymptomatic P. falciparum infections but not in clinical malaria cases, where gametocyte carriers were more frequently detected by microscopy among subjects with lower parasite densities. In P. vivax infections, the level of gametocytes mirrors the asexual parasite density, both in symptomatic and asymptomatic infections. In endemic areas, patent P. falciparum infections were approximately three times more infectious than submicroscopic infections. Mosquito membrane feeding assays conducted in four African countries showed that the likelihood of mosquito infection is very low at gametocyte densities below one parasite per microliter and increases steadily from ten parasites per microliter. Therefore, the importance of asymptomatic infections compared to clinical malaria cases in P. falciparum transmission depends on asexual and sexual parasite densities, whereas the relative contribution to the infectious reservoir in a given setting depends on the frequency of asymptomatic infections in the population. Tadesse concludes stressing the importance of conducting longitudinal studies to assess the impact of different factors on parasite biomass kinetics and infectivity.
Plenary Session II COVID-19: Lessons Learned and Future Challenges
Anthony Fauci (National Institutes of Health, United States) started the session with a comprehensive overview of the basic aspects of the SARS-CoV2 infection: virology, transmission, clinical presentation and manifestations of severe COVID-19 disease, social determinants of risk, fundamental public health measures, and therapeutics and vaccines. He described COVID-19 as a pandemic that reached historical proportions not seen in the last hundred years. Fauci further mentioned that if adherence to the main public health response strategies were higher, we would not have seen a resurgence as dramatic as currently happening in the United States and Europe. Towards the end, Fauci described recent events in vaccine development and said he is optimistic that first doses will be administered to priority groups before the end of this year.
John N. Nkengasong (Africa Centres for Disease Control and Prevention, Ethiopia) presented an overview of the COVID-19 response in Africa. The joint continental strategy was preventing transmission, death, and social and economic harm. He named several partnerships and initiatives that played a critical role in the response, such as the partnership to accelerate COVID-19 testing (PACT) in Africa. He further described epidemiological trends across African countries, which increasingly show concerning trends starting in the second half of the year. Key features in Africa’s response to COVID-19 were unified leadership, along with a new public health order, partnerships, adaptive development and allocation of public health workers as well as investment in local manufacturing of medical interventions. As the way forward, he emphasized the need to maintain the gains achieved and to be prepared for the second wave in Africa by intensifying public health and social measures against COVID-19, including scale-up of testing and surveillance.
‘The lessons are yet to begin’ was the cautious introduction of Heidi Larson (London School of Hygiene and Tropical Medicine, UK) in her talk on “COVID-19: Lessons Learned and Future Challenges”. She presented results from the Vaccine Confidence Project, which demonstrate the importance of confidence in products, providers, policymakers, and public health systems, in the public’s willingness to accept a vaccine. Larson mentioned a wide variety of factors that would contribute to low acceptance and described vaccine hesitancy as a challenge not only in subgroups but also in the wider population. According to Larson, misinformation would be a serious obstacle to the acceptance of a COVID-19 vaccine and could be a ‘tipping point phenomenon’ towards achieving coverage levels required for herd immunity.
In the final talk of the session, Richard Hatchett (Coalition for Epidemic Preparedness Innovations – CEPI, United Kingdom) gave an overview of the role of CEPI in COVID-19 vaccine development and access. In partnership with the leading COVID-19 vaccine developers and non-governmental organizations, CEPI supports funding of nine vaccine candidates, eight of which are in clinical trials. Hatchett described various projects of CEPI that aim to ensure ‘global access to vaccines to all countries at the same time regardless of income’ and current efforts as well as challenges to achieving that goal. In the outlook for the future, Hatchett mentioned that CEPI aims to deliver two billion doses around the world in 2021, and emphasized the need for better preparedness plans for the next pandemic and Disease X, for which their strategy could serve as a model.
Symposium #7: Human Landing Catches: Alternatives and Directions for the Future
As symposium organizers, Sarah Zohdy (Centers for Disease Control and Prevention, United States) and Jenny S. Carlson (United States Agency for International Development, United States) described human landing catches (HLC) and other mosquito collection methods for entomological surveillance and discussed imitations and challenges including standardization.
Heather Ferguson (University of Glasgow, UK) talked about the evaluation of the mosquito electrocuting trap (MET) in a region of Burkina Faso. Although METs caught 40-50% fewer An. gambiae mosquitoes than HLC, they provided a consistent representation of vector dynamics, species composition, biting behavior and infection rate. Therefore, despite limitations in sensitivity, METs could be a useful alternative collection tool. METs were also evaluated compared to BG-Sentinel traps for Aedes catches, with no significant difference between the two methods. However, the trial had limitations and more work for full evaluation was recommended. Challenges of METs were discussed and the development of a MET product following the identification of country-specific needs was envisaged.
Nicodem J. Govella (Ifakara Health Institute, Tanzania) presented on the success of MET as an alternative to HLC for Anopheles surveillance. The target product profile used to develop METs was aimed at mimicking the set-up for HLC with no risk of exposure by the user and was tested for safety, quality and efficacy. Optimization was conducted as to the exact power needed to kill the mosquitoes while leaving them intact, after which the first trial was conducted in rural Tanzania. A sensitivity of 58% indoors and 20% outdoors, and a similar estimate of mosquito behavior relative to HLC was observed. Improvement of METs prior to the second trial in urban Tanzania resulted in better performance. The applications of METs included investigation of biting time and distribution of biting between indoor and outdoor environments in an experiment carried out in the Kilombero Valley, Tanzania. Moreover, MET was used to survey malaria vectors nationally and to assess how outdoor exposure to malaria vectors varied across diverse ecological settings of transmission in Tanzania in both dry and wet seasons over 3 years.
Krijn Paaijmans (Arizona State University, United States) talked about human-baited traps as an alternative to HLCs to accurately evaluate key medical entomological parameters with a caption on “Nothing more attractive than a human”. Paaijmans described humans as excellent mosquito lures, pointed out the effectiveness of LLIN acting as a lethal lure in case of no resistance and highlighted the shortcomings of the human landing catches and why they should not be used. He talked about the Mozambican Alliance Towards Elimination of Malaria (MALTEM) project, which used the Centers for Disease Control and Prevention light trap (CDC light trap) deployed within human-baited tent traps indoors and outdoors. They generated evidence in Maputo province, Mozambique, to help the national malaria programs to design elimination strategies with significant achievements in Gaza and Inhambane. Paaijmans ended talking about the current development of next-generation human-baited tent traps.
Frances M. Hawkes (University of Greenwich, United Kingdom) introduced HLCs and their use for understanding mosquito biting behaviour in malaria pre-elimination settings and presented data on how HLCs might systematically under-estimate biting rate. She presented the findings obtained using the host decoy traps (HDTs) for outdoor malaria vector surveillance which caught ten times more An. gambiae than HLC in Burkina Faso and Benin. Based on social and operational acceptability of the HDT, additional research was conducted across different settings in both highlands and lowlands. They also carried out qualitative assessments through interviews and focus group discussions to understand community responses to HLC. Field volunteers perceived HLCs as risky and difficult, associating it with disease and negative impact on their activities due to exhausting night work.
Brian D. Foy (Colorado State University, United States) presented on human-baited tent traps for sampling host-seeking malaria vectors in West Africa. The traps were tested in Malabo, Equatorial Guinea and in Senegal with satisfactory results compared to other catching methods. The human-baited tent traps did not result in exposure to any vector-transmitted disease since no mosquito bites occurred in the process of catching. Foy gave a brief discussion on the advantages and disadvantages of human-baited tent traps with battery-powered trapping signs. Foy ended talking about the RIMDAMAL trials I and II that assess the efficacy and risk of harm of repeated ivermectin mass drug administration (MDA) for malaria control.
John Gimnig (Centers for Disease Control and Prevention, United States) presented an overview of HLC, which remains the gold standard in entomological monitoring. Despite their shortcomings, human bait catches remain the most useful single method of collecting anthropophagic mosquitoes because there exists no replacement attractant for humans. Gimnig pointed out what could be learned about the biting behavior of the mosquitoes and the supplementary outcomes using HLC. He presented a pooled analysis for comparing trapping methods, identifying the different replacements for HLC with the CDC light trap indoors being the safest. He reviewed the analyses carried out on mosquito indoor and outdoor biting behavior with data from An. funestus biting times collected from different sites. Lastly, Gimnig emphasized the disadvantages and limitations of HLCs.
Symposium #19: Mechanistic Dose-Response Modelling of Antimalarial Drugs
Joel Tarning (Mahidol Oxford Tropical Medicine Research Unit, Thailand) presented a study on pharmacokinetics (PK) and mosquito-killing effects of ivermectin and its metabolites. Ivermectin showed potent mosquito-killing effects when the mosquitoes (Anopheles dirus and A. minimus) fed on blood from humans who had taken ivermectin, both in membrane feeding and direct feeding assays. Two clinical trials in human volunteers were pooled and analysed using a population PK modelling approach. Bodyweight and co-administration of dihydroartemisinin-piperaquine showed a significant impact on the pharmacokinetic properties of ivermectin. Predicted drug concentrations of ivermectin and its metabolites were linked to mosquito-killing effects and showed substantial differences between mosquito strains. Modelling and simulation suggest potent mosquito-killing effects for over 7 days after a standard 3-day oral dose of ivermectin. The developed model could be a valuable tool to inform dosing policy on transmission blocking and malaria elimination efforts.
Palang Chotsiri (Mahidol Oxford Tropical Medicine Research Unit, Thailand) presented on the topic “Primaquine pharmacokinetics and pharmacodynamics (PK/PD) modelling”. Primaquine is an effective drug for treating P. vivax because of its activity on liver stage parasites. Chotsiri’s presentation showed a population PK/PD modelling approach to predict PK properties of primaquine, and its effect on gametocytes and mosquito infectivity. In the gametocyte dynamics model, Chotsiri showed that primaquine killed gametocytes and higher doses of primaquine resulted in a shorter time to eliminate gametocytes from the blood. Mosquito infectivity was affected by both primaquine and gametocytes, resulting in a lower infectivity at low gametocyte density and high primaquine concentrations. Taken together, this model could be used to determine an optimal primaquine dose for blocking transmission of malaria.
Karen Barnes (University of Cape Town, South Africa) gave a talk focused on improving malaria treatment in vulnerable sub-populations (i.e. pregnant women, infants, hyperparasitaemic patients, or individuals with co-morbidities), which represent an important share of all malaria cases. Antimalarial drugs must be given at optimal dosages to ensure that all patients have an equal chance of being cured; however, during clinical drug development, vulnerable populations are usually excluded. Pooling already existing PK data and conducting individual patient data (IPD) meta-analyses can help to establish adequate dosages in these populations, achieving a sufficient sample size to reach the statistical power needed and increasing validity and generalizability of findings. Currently, this approach is being used to investigate artemisinin combination therapies (ACTs) for treating malnourished children with malaria. Malnourished children were observed to have an increased risk of delayed parasite clearance, recrudescence and re-infection, suggesting suboptimal dosing in this vulnerable population.
Julie Simpson (University of Melbourne, Australia) highlighted the significant declines in efficacy of ACTs in the Greater Mekong Subregion. Using within-host malaria models that capture the interplay between drug concentration and action, the efficacy of combination therapies can be predicted, providing a clinical decision tool for selecting dosing schemes and combination therapies for current and new antimalarials to be evaluated in clinical trials. One case study example is triple ACT (TACT), which combines dihydroartemisinin (DHA) + piperaquine (PPQ) + mefloquine (MQ). An in silico model was used to determine the optimal TACT dosing regimen to achieve ≥90% 42-day cure rates in regions where parasite resistance to DHA-PPQ has emerged. The model predicted the cure rates observed in the TACT clinical trials and is available as an online clinical decision tool (TACT R Shiny App, www.qmalaria.org). Another case study example presented was within-host malaria modelling of the combination therapy OZ439-DSM265, using data from volunteer infection studies, which demonstrated an antagonistic interaction of the combined effect of OZ439-DSM265 and determined the minimum optimal dosing regimens required to achieve a 42-day cure rate ≥90%.
Symposium #20: A Fundamental Way to Prevent Malaria in Pregnancy: Improving Health Outcomes for Pregnant Women and Their Babies One Nurse and Midwife at a Time
Katherine Wolf (Jhpiego, United States) as a symposium organizer highlighted the fifth anniversary of the IPTp Call to Action. While progress has been made, the call is being renewed, particularly as the world faces the COVID-19 pandemic. Health continuity is critical, particularly for expectant mothers in malaria endemic areas. Wolf noted that nurses and midwives are adapting the care they give to pregnant women during COVID-19 to ensure that no pregnant women experience malaria. She invited participants to join the IPTp Call to Action.
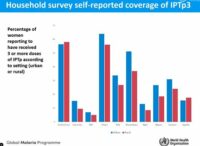
Pedro Alonso (World Health Organisation, Switzerland) presented the WHO approach to speed up and scale up the fight against malaria in the pregnant women. WHO’s three-pronged approach is encouraged during pregnancy; including the use of insecticide-treated bed nets to avoid women/vector contact, uptake of sulfadoxine-pyrimethamine (SP) and antimalarial preventive treatment and access to prompt diagnosis and effective treatment. Since 2010, an overall improvement was noted in the number of women who attend antenatal care (ANC) at least once and received malaria intermittent preventive treatment for pregnancy (IPTp). However, there are still barriers, such as transportation, level of education and wealth, which render unacceptable the level of ANC and IPTp coverage. Pregnant women cannot be considered as a forgotten group but a key vulnerable group. Thus, WHO is committed to continuing to put them at the centre of their fight against malaria.
Maud Lugand (Medicine for Malaria Venture, Switzerland) presented on quality measures used in manufacturing medicines used for intermittent preventive treatment for malaria in pregnancy. IPTp is a WHO-recommended intervention, which involves administration of a course of sulfadoxine-pyrimethamine (SP) at each antenatal care visit from the second trimester of pregnancy, as Alonso mentioned before. Its uptake is very low despite being an effective intervention; in 2018, only one third of eligible women in Africa were optimally protected. Sociocultural barriers for low uptake include medical pluralism, low patient acceptance and self-medication. Structural barriers included limited access to ANC services, non-availability of quality-assured SP and low health provider acceptance. MMV supported building GMP production capacity in the region in Nigeria and Kenya, and is currently in the process of developing a user-friendly IPTp-SP package to support local manufacturing companies. They field-tested the packaging to ascertain the use and acceptability, knowledge and perception of it. Results showed women and health care providers had positive experiences with the package.
Aissata Fofana (RTI International, Guinea) shared a study on bringing long-lasting insecticidal nets (LLIN) distribution closer to communities in Guinea through adaptive management, called StopPalu+. This project is to assist the government in reducing malaria-associated morbidity and mortality by helping increase LLIN distribution in the country through monitoring and evaluation. They discovered that distribution points were far and households lost their vouchers for net distribution, therefore the data collected was used to implement the following adaptation measures. Communities were split closer to distribution points, radio spots were used to encourage people to provide their names to get a copy of a voucher for an LLIN, and sensitization activities in schools and group discussions with women and youth associations were held. All these interventions helped increase the expected coverage of LLINs by 20%.
Yacouba Ouedraogo (Jhpiego, Burkina Faso) presented a pilot study on testing the feasibility of community-based IPTp (C-IPTp) provision in Burkina Faso. At only 17-22%, IPTp coverage was low in Burkina Faso in 2014 and 2015, calling for a high-impact intervention to improve the situation. The study explored whether a community-based approach combined with promotion of routine ANC could increase IPTp coverage. Four health facilities in three districts with high malaria transmission were selected; with baseline and endline surveys conducted, in which the intervention was carried out by community health workers, who were trained and supervised by nurses. IPTp coverage was monitored, and results show an increase in ANC and IPTp4 in both intervention and control groups with IPTp3 and IPTp4 respectively at 50% and 22% in the control versus 64% and 49% in the intervention group at endline. However, no significant difference between controls and interventions was detected. The study revealed that community health workers (CHW) could be trained to provide C-IPTp and is still being implemented in some districts in Burkina Faso.
Jenipher Mukolwe Angaha (Jhpiego, Kenya) shared results from a study in Nigeria and Kenya on the effect of group antenatal care (G-ANC) versus individual ANC on IPTp and ANC attendance. During this study, G-ANC was embraced by both women and health care providers based on many aspects like patient-provider relationship, organisation of care, engagement and empowerment of women. It resulted in increases in ANC attendance and experience of care for women providers and supported further studies on G-ANC to improve coverage of other interventions. The study found the mean number of IPTp doses received was higher for the intervention arm compared to the control arm (Nigeria: 3.45 versus 2.14, p < 0.001; Kenya: 3.81 versus 2.72, p < 0.001).
Symposium #24: Aedes Surveillance in Africa: (Re-) Building Capacity to Address Growing Arboviral Disease Threats
In her talk on “Aedes-borne arboviruses as an emerging public health threat in Africa and multi-sectoral approaches for prevention and control”, Florence Fouque (Special Programme for Research and Training in Tropical Diseases from the World Health Organization, Switzerland) highlighted the worrying re-emergence of arboviral diseases in Africa. Thus, severe surveillance and control networks have been set up against these often understudied diseases in Africa. To effectively do this, the study’s main objective was to develop a reference and workable framework for the application of the multisectoral approaches in controlling vector-borne diseases (VBDs), identifying the best path to take in future collaborations among different sectors. The main findings demonstrated the effectiveness of a multisectoral approach in entomological surveillance to provide guidelines for the successful control and elimination of Aedes alongside other VBDs.
Presenting on “The West African Aedes Surveillance Network (WAASuN)”, Samuel K. Dadzie (Noguchi Memorial Institute for Medical Research, Ghana) noted the need to have a surveillance system on the Aedes vector since reports have recorded arboviral diseases in 34 African countries. Increased surveillance would provide essential information and adequate preparedness against Aedes-borne parasites. Therefore, WAASuN was established in Sierra Leone in 2017 to enhance collaboration on Aedes surveillance between West African countries. So far, this network has successfully trained over 60 participants in insecticide resistance monitoring and geomapping, establishing good collaborations with international health organizations such as the Special Programme for Research and Training in Tropical Diseases from the World Health Organization (WHO/TDR), Centers for Disease Control and Prevention (CDC), Partnership for Increasing the Impact of Vector Control (PIIVEC), West African Health Organization (WAHO) and Emory University, among other achievements. Future prospects aim to further strengthen this collaboration and extend the network to cover the entire African region.
Rebecca S. Levine (Center for Disease Control and Prevention, USA) while addressing the capacity of entomological surveillance in Sierra Leone, pointed out the little attention paid to Aedes-borne viruses in Africa. One reason is that these viruses constitute greater public health threats for immunologically-naïve non-African human populations. Secondly, the magnitude of the burden of malaria and many neglected tropical diseases in Africa detract attention from Aedes-borne infections. Over the years entomology capacity in Sierra Leone has greatly improved, as insecticide-treated bed nets (ITNs) distribution (2006), indoor residual spraying (IRS) trials (2010-2012), and the establishment of the IVM task-force (2016) monitoring insecticide resistance are important milestones in vector control activities in the country. This culminated in 2017 by the launch of the surveillance of Aedes aegypti in West Africa by the CDC and Emory University and the creation of the WAASuN. In 2018, under the USAID/CDC President’s Malaria Initiative (PMI), monthly entomological monitoring and vector control interventions (ITN, IRS) were conducted. A partnership between the PMI and the Aedes project was hence established. With a budget of 16000 USD, the 12-month project began with sample collection in October 2019. Unfortunately, the COVID-19 pandemic has been a major impediment to the study. Notwithstanding, this project ultimately promises to bring to light the status of the Aedes population in the region.
Mawlouth Diallo (Dakar Institut Pasteur, Senegal) gave a detailed account of the Aedes surveillance system in Senegal. The programme objectives were to characterize the vectors and study their biology and ecology, to identify the vertebrate hosts and establish the transmission cycle, and investigate .the efficiency of vectorial transmission (vector competence, vector heterogeneity and distribution, virus-vector-host interaction dynamics. The research took a multidisciplinary approach, targeting the entomology, virology, and host (human/non-human primate) aspects in Aedes-borne arboviruses surveillance. Preliminary data showed a difference in the Aedes mosquito behavior in Africa compared to non-African regions of Asia and America. There was also a notable increase of insecticide resistance which needs to be closely monitored. Important to note was the fact that Aedes mosquitoes are governed by different conditions compared to Anopheles species, and the use of malaria vector control strategies as a reference point for Aedes control might not be as effective. New tools for vector control need to be developed, including increasing the capacity for vector surveillance at the district and community levels.
This report is brought to you by the MESA Correspondents. Senior editorial support has been facilitated by the Organizers and Co-Chairs of the symposia, Valentina Mangano (University of Pisa) and Julie Chaccour (Independent Consultant). This report is cross-posted on the MESA website and on MalariaWorld.
Published: 18/11/2020
This report is brought to you by the MESA Correspondents Busari Lateef Oluwatoyin, Jaipal Singh, Nathalie Amvongo Adjia, Manuela Runge, Ivan Mbogo, Núria Balanza, Nutpakal Ketprasit, Rebecca Pwalia, Lilian Mbaisi, Ntui Vincent Ntui-Njock, and Jenna Zuromski. Senior editorial support has been facilitated by the Organizers and Co-Chairs of the symposia, Valentina Mangano and Julie Chaccour.
THEMES: Basic Science | Epidemiology | Health Systems