Last Updated: 22/12/2016
Understanding human, parasite, vector and environmental interactions driving residual malaria transmission in Papua New Guinea
Objectives
To investigate the prevalence of ongoing malaria transmission and to determine how humans, vectors and their interactions influence human infection by malaria in two sites in Papua New Guinea.
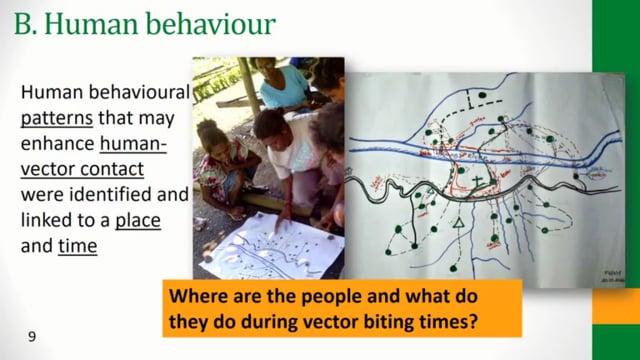
This research proposal aims to address this knowledge gap by conducting detailed investigations of (1) prevalence and distribution of malaria infection to confirm/identify/update the magnitude of residual malaria at the time of study, (2)vector studies to characterize the local vector population abundance, composition and behaviour, as well as their determinants, (3) Investigation of the mosquito-human contact patterns and tracing routes of transmission, (4) human behaviour, in order to understand what behaviour renders which population groups susceptible to residual transmission, and (5) the establishment of a clinical surveillance system linked to geo-referenced village locations in order to validate a routine system for identifying focal areas of transmission. Understanding the extent of local heterogeneity in malaria transmission and the driving factors is critical to be able to identify and implement targeted control strategies to ensure the ongoing success of malaria control in PNG.
Papua New Guinea Institute of Medical Research (PNG IMR), Papua New Guinea
The scale-up of malaria control intervention in PNG has resulted in a significant overall reduction in the nationwide prevalence and incidence of malaria. However, this effect has not been uniform across the country and considerable differences in transmission exist in different areas, despite a standardised approach to the implementation of the control measures. Limited data currently exist on the factors that determine these differences and residual malaria transmission in PNG. Human, vector and/or parasite behaviour/characteristics are the most important obstacles to elimination.
This study involved:
- Village census and household prevalence surveys;
- Establishing clinical surveillance system to collect information on the number of patients presenting to health facilities with malaria-related fever;
- Constructing maps of malaria incidence and prevalence to identify key transmission areas;
- In-depth interviews and focus group discussions to collect data on human behaviour relating to vectors and transmission;
- Larval and mosquito collection and analysis.