Last Updated: 30/07/2024
Integrating molecular surveillance for P. falciparum elimination: a tool for the national and local malaria control programs in international borders of Brazil
Objectives
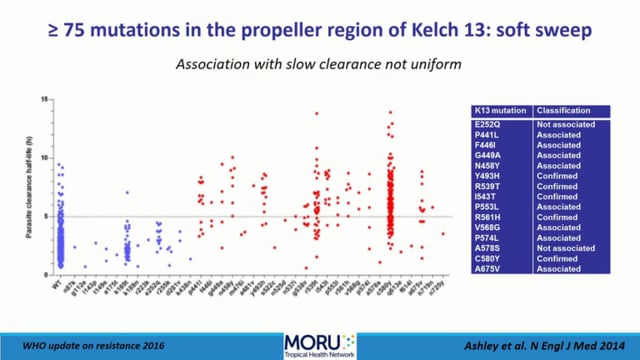
The approach in this project involves development of a molecular malaria surveillance tool to monitor drug resistance to P. falciparum using Kelch 13, PfCRT, PfMDR genes and deletion of PfHPR2 and PfHPR3, thereby supporting public-health systems to tailor interventions to sustain control and reach (pre)-elimination stages.
Andrea Regina de Souza Baptista
Joseli de Oliveira Ferreira
Ricardo Luiz Dantas Machado
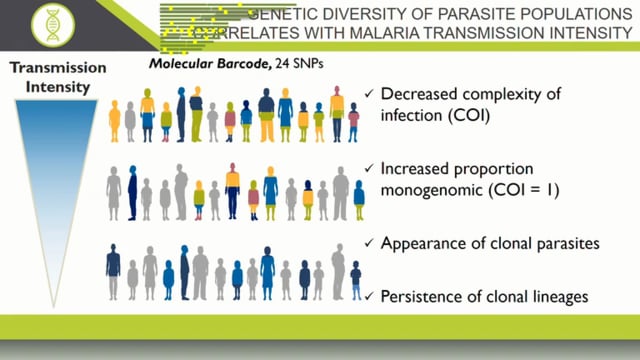
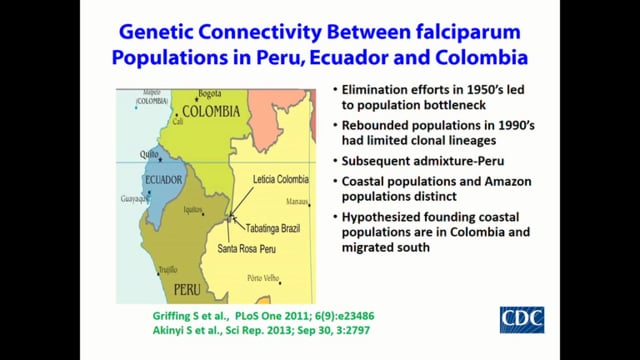
In 2016, Brazil launched its National P. falciparum Elimination Plan (BNEP) based on the achievements acquired in recent years, after scale up interventions including the introduction of artemisinin-based combination therapy (ACT) and free LLINTs in endemic areas. Data from the National Malaria Control Program (NMCP) of the Ministry of Health (MoH) showed that in 2016, of 808 municipalities of the Amazon region, 514 did not have P. falciparum transmission in the last three years, but the other 294 municipalities had Annual Parasitic Incidences (API) between low and high epidemiological risk. The BNEP is based on early diagnostic tools, opportune and adequate treatment, improvement surveillance, health education and vectorial control activities. Important focus is given in international borders, indigenous and gold mining areas. The increase in imported malaria from countries bordering Brazil has been an important concern for the elimination of P. falciparum. Effective surveillance of the parasite population in the emergence and spread of new genetic variants and monitoring of parasite migration are pre-requisites for disease elimination. The goal of the BNEP is to eliminate P. falciparum malaria before the emergence of ACT resistance. There is a growing threat of the emergence and spread of artemisinin resistance, first reported in Southeast Asia, but recently in Guyana and Suriname, near the border with Brazil. Both case reports provide evidence of the serious risk that artemisinin resistance spreads or/and emerges independently in other countries in the Americas. Tracking drug resistance will be essential to prevent the spread of artemisinin resistance, which would seriously undermine malaria elimination efforts. Usually, to study the efficacy of antimalarials, WHO recommends the realization of clinical trials that are time-consuming, and results are slow to be available to decision makers. On the other hand, several studies are showing an increasing proportion of deletions of the Pfhpr2 gene, and its structural analogue Pfhpr3, which are important for the detection of P. falciparum in Rapid Diagnostic Tests (RDT). With today’s technological advances, methods for genome sequencing have become affordable and much cheaper, making easier epidemiological and genomic studies. In addition, new techniques allow sequencing the parasite of malaria from small volumes of blood (digital puncture). Genomic information and genetic diversity of parasites, together with the epidemiology data can be used to monitor transmission, emergence and spread of drug resistance and the effectiveness of diagnostic methods and control interventions. In this way public health systems can be supported to maintain control of malaria cases and to reach a phase of elimination more quickly. The proposal sets to develop a P. falciparum molecular surveillance system (MSS) for support the national elimination program. This Pf-MMS will be interconnected with the National Epidemiological surveillance system used in Brazil from 2003.
Jan 2023