Last Updated: 14/06/2024
Enhanced Active Surveillance: Establish mechanisms for serology-based epidemiological surveillance
Objectives
Primary Objective:
To establish a serological surveillance system to identify malaria-exposed individuals to aid the targeting of malaria elimination strategies.
Secondary Objective:
- To determine the usefulness of serology as a tool that is integrated into the National malaria surveillance program
- To identify the operational challenges in implementing serosurveillance in the National program
- To determine the long-term sustainability and financial feasibility of serosurveillance
National Institute of Malaria, Parasitology and Entomology (NIMPE) Vietnam, Vietnam
Background:
Serology is a common surveillance tool for a wide range of infectious diseases. Cross sectional surveys and prospective cohort studies can be used to monitor changes in disease exposure at a population and individual level. Malaria surveillance however, has generally only measured current infection or entomological parameters, with the former focusing on rates of parasitaemia measured by light microscopy, rapid diagnostic tests and nucleic acid amplification. Each of these approaches may have limitations in precision, sensitivity, time-costs, required technical expertise, throughput, and financial costs. Seroepidemiology is increasingly recognised as cheap, low cost approach that can also provide highly sensitivity detection of recent parasite infection in symptomatic and asymptomatic individuals. Simple blood collection from finger-prick samples means that sampling can be rapid and non-invasive. Antibodies can be measured by ELISA-based methodologies that are high-throughout, low cost and can be performed locally.
Project Overview:
Even sensitive detection methods like nucleic acid amplification may fail to detect individuals exposed to Plasmodium infection because of limitations in sensitivity and frequency of testing. Immunological responses however, are acquired even with infections of low parasitaemia. Immunological responses remain detectable for weeks to months and thus can be used as a highly sensitive tool to detect parasite exposure over a preceding block of time, and not just reflecting current infection.
This activity will build upon the sample collection system outlined in Activity 4.1 and will develop capacity to undertake serological testing for a range of malaria antigens at NIMPE. Although this approach is well established as a research tool, it needs to be evaluated as a strategy that is integrated into a National surveillance program and to determine its usefulness in guiding malaria elimination responses. This will provide a new tool to track changes in exposure at a population level over time and monitor the impact of malaria elimination interventions. It has also been demonstrated that these immunological responses can indicate the susceptibility of a population to severe and symptomatic malaria and may be used as an early indicator of risk should malaria be re-introduced into a region. The approach may also be expanded into serosurveillance for vaccine-preventable diseases and other common infectious diseases.
Project Methodology
Importantly it utilises samples from all patients tested for malaria infection (i.e. malaria negative as well as malaria positive) so that serological outcomes can also be assessed for people with subpatent infections. From 2016, the technical methods for indirect ELISA for malaria antigens will be transferred to the NIMPE laboratory staff. Serosurveillance data will be integrated into the SDSS to identify associations between serological dynamics and disease transmission. The SOPs will be defined in collaboration with Burnet Institute at the start of the implementation period.
Samples will be stored at 4oC at the Provincial level, until transferred to NIMPE. At NIMPE, these DBS will be stored at -20oC until required for batch testing. At that time DBS will be extracted using procedures that will be defined SOPs, and then tested by indirect ELISA, again using defined SOPs. Samples will be identified by a unique barcode.
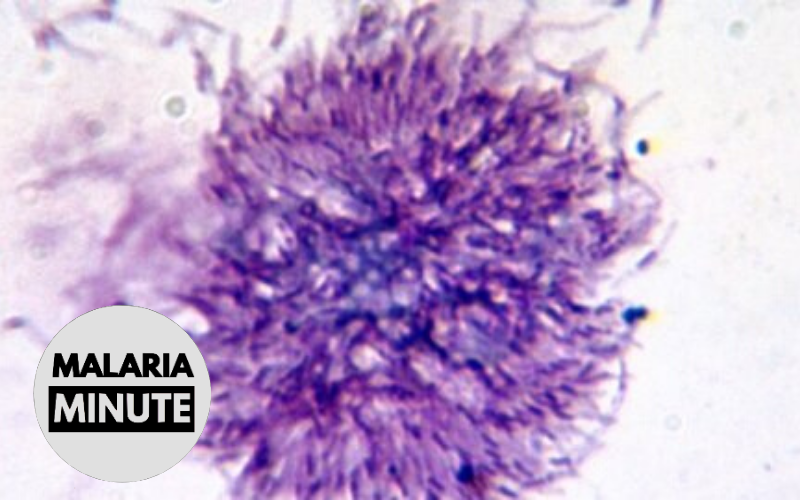
DBS samples will be used to elute antibodies at the laboratories in NIMPE. These antibodies will then be used to detect reactivity against a range of malaria antigens. This will include antigens that are highly immunogenic and are known to be induced after few infections, and antigens that are less immunogenic and that require multiple exposures to malaria infection. They will also include antigens that are known to induce long-lived antibody responses and therefore reflect exposure over prolonged periods of time and antigens that have short lasting responses and therefore reflect recent exposure to malaria infection. Antigens will be selected from the following: pre-erythrocytic antigens including CSP, merozoite surface proteins including MSP1, MSP2, MSP3, EBA175, EBA140, and Rh proteins.
Oct 2015 — Dec 2016