Last Updated: 27/05/2025
Epidemiology and determinants of emerging artemisinin-resistant malaria in Ethiopia
Objectives
To improve current understanding of the epidemiology and drivers of emerging artemisinin resistance in the Horn of Africa and produce tools that can be used by malaria programs to identify, predict, and respond to emerging drug-resistant strains in Africa.
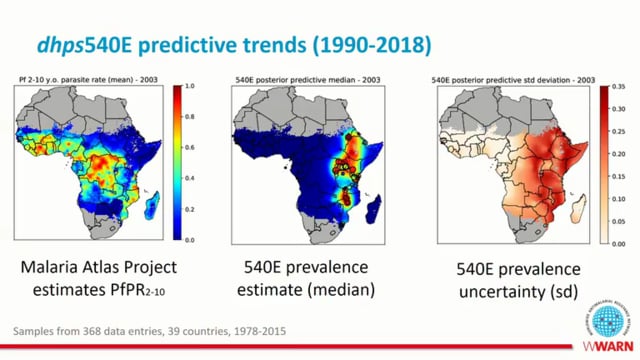
Plasmodium falciparum strains with resistance to first-line artemisinin-combination therapies (ACTs) threaten malaria control and elimination efforts across Africa, where 95% of the world’s malaria cases and deaths occur. Artemisinin resistance is mediated by mutations in the pfkelch13 (K13) gene that have only recently impacted the region. Concerning K13 mutations have now been confirmed in Africa, including emergence and expansion of the candidate artemisinin-resistance K13 R622I mutation in the Horn of Africa (HoA). Increasing reports from the HoA by us and others also indicate that “diagnosis resistant” strains that escape detection by widely used rapid diagnostic tests due to deletions of the histidine-rich protein 2/3 (pfhrp2/3) genes are now established across the region. The dual emergence of drug and diagnostic resistance mutations threatens frontline test- and-treat strategies and may have profound impacts on malaria control. Improved understanding of the determinants of infection by R622I parasites is needed to inform clinical practice and policy decisions. In collaboration with the Ethiopian Public Health Institute, the technical arm of the Ethiopia Federal Ministry of Health, and leading academic partners, surveys of people presenting to health facilities with falciparum malaria across Ethiopia will be conducted to achieve the following Aims. Aim 1 will elucidate risk factors for infection by artemisinin-resistant P. falciparum, including whether the presence or absence of pfhrp2/3 deletions impacts risk. A clinical risk tool will be developed to help predict who may be infected by an artemisinin- resistant parasite. Such a tool could be used for targeted implementation of antimalarial treatment options designed to overcome resistance and prevent its spread, such as triple ACT that employs two partner drugs alongside an artemisinin derivative. Aim 2 will determine the impact of K13 R622I on drug resistance and parasite fitness in pfhrp2/3-deleted and intact parasites. Aim 3 will develop a predictive model of the future spread of artemisinin resistance within and out of the HoA, focusing first on development of data/models of human and parasite migration and then integrating in vivo data from Aim 1 and in vitro data from Aim 2.
Jun 2023 — May 2028
$3.59M